The Female TRT Backlash: Why Some Doctors Still Refuse to Prescribe
Published on:
Updated on:
People are asking...
It seems like its very difficult for many people to get a PCP to write a prescription for testosterone. Is this because there is greater risk of malp...
This is true about the challenging nature of getting a PCP to sign off on TRT, but not for those reasons. TRT is one of the safest treatments out there with one of the lowest malpractice insurance rat... See Full Answer
Do you treat women? And would admitting I've been taking small amounts [10-20mgs/week IM] of my bf's Test (and getting great results) be a barrier to...
We currently have female patients on similar low doses to optimize their hormones. They typically need a bit of Estrogen to keep everything in balance as well as the Test, and to be monitored a bit mo... See Full Answer
Do you foresee patients currently dependent on TRT to sort of be “screwed” at any point due to increased regulations that make it so they can no longe...
I don’t have a crystal ball, but I don’t see that being a problem. Treatment is becoming more prevalent because we are better at recognizing the symptoms, more open about talking about it, and recent ... See Full Answer
Have a question? Ask us.
At AlphaMD, we're here to help. Feel free to ask us any question you would like about TRT, medical weightloss, ED, or other topics related to men's health. Or take a moment to browse through our past questions.
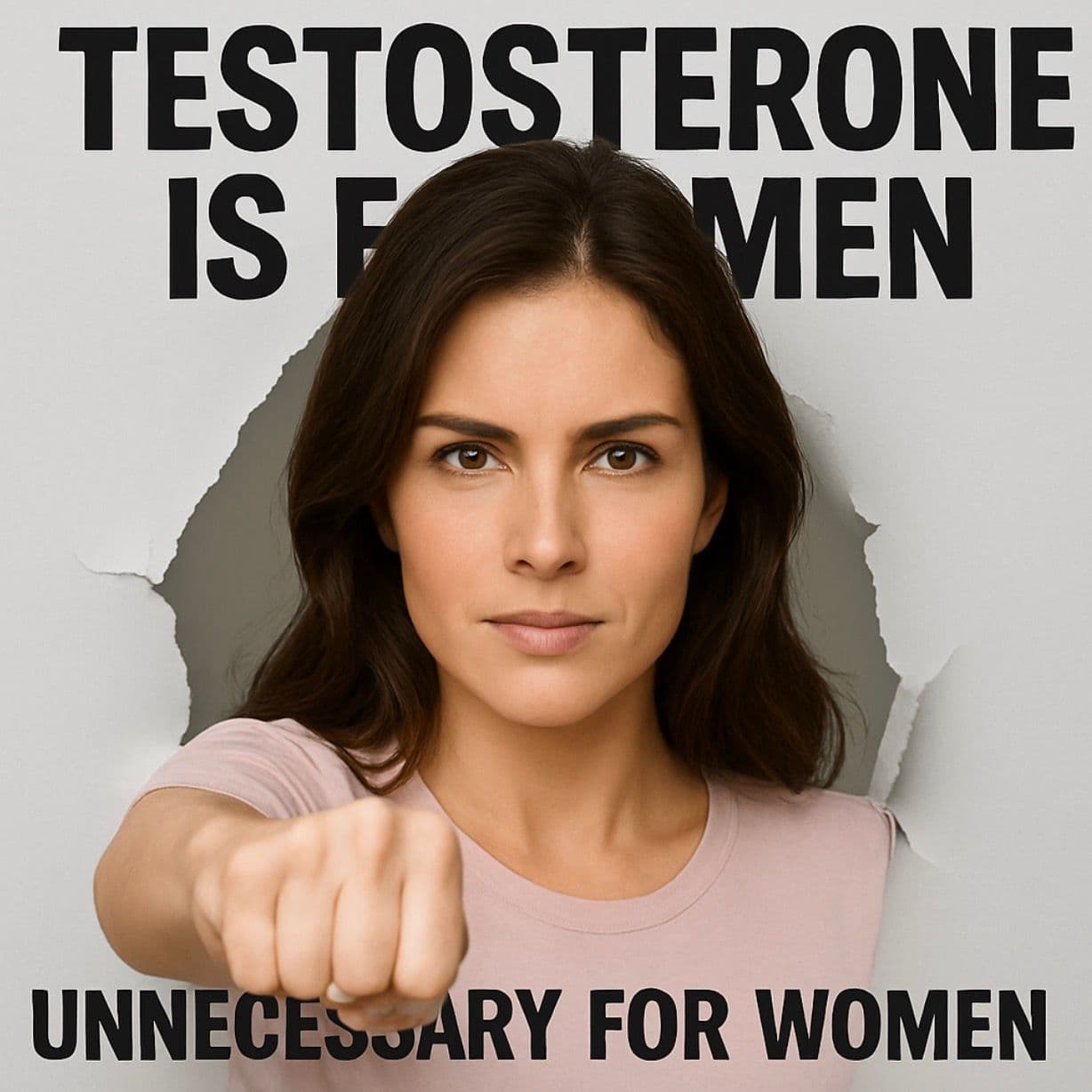
Testosterone therapy for women is one of the most misunderstood—and often dismissed—topics in modern medicine. While research and real-world results show its benefits for energy, mood, sexual health, and overall well-being, many women still encounter a frustrating roadblock: a doctor who refuses to even consider it.
The question is… why?
Outdated Medical Views Die Hard
Historically, testosterone has been labeled a “male” hormone. That label has shaped decades of medical education and patient care. The truth? Women produce testosterone naturally in smaller amounts than men, and it plays a critical role in muscle mass, bone density, mental clarity, and libido.
Yet many doctors were trained in a system where:
- Testosterone in women was ignored or viewed only in the context of illness.
- Female hormone health was narrowly focused on estrogen and progesterone.
- “Normal” lab ranges for women were based on outdated reference points, often from women in their reproductive peak—not accounting for age-related decline.
This bias continues to influence treatment decisions today, leaving women without the care they need.
Real Stories from Women Who Refused to Accept “No”
At AlphaMD, we hear these stories far too often:
- Sarah, 47, went to her doctor after months of exhaustion, low libido, and brain fog. Her labs showed testosterone levels barely detectable. She was told, “You don’t need testosterone—you’re a woman.” After connecting with a provider who understood female hormone balance, Sarah began low-dose TRT and felt like herself again within months.
- Dana, 38, was told by three separate doctors that her symptoms were “just stress.” When she mentioned low testosterone, one physician actually laughed. She later found a clinic familiar with female TRT, where her levels were finally tested and addressed.
- Maria, 55, had a hysterectomy years ago and noticed a sharp drop in energy and mood. She requested testosterone testing and was told it “wasn’t relevant.” She found AlphaMD’s educational resources, learned the right questions to ask, and ultimately began a carefully monitored treatment plan that changed her daily life.
These aren’t rare. They’re part of a larger pattern where women must become their own advocates to receive comprehensive hormone care.
Why the Medical Resistance Persists
Even with growing evidence, resistance remains because:
- Medical training lags behind current research – Many providers still rely on outdated hormone replacement models focused only on estrogen and progesterone for women.
- Fear of liability – Without FDA-approved testosterone products for women in the U.S., some doctors avoid prescribing it altogether.
- Persistent myths – Concerns about side effects like voice changes or heart issues are often based on outdated, high-dose studies—not the carefully monitored, physiologic doses used today.
The Shift Has Started—But Slowly
Forward-thinking physicians and hormone specialists, including those who partner with AlphaMD, are working to close this gap. They use evidence-based protocols, precise dosing, and regular monitoring to restore women’s testosterone to healthy levels—helping them reclaim energy, mood, and vitality.
Women are also finding strength in numbers. They’re speaking out, joining online communities, and using trusted resources to share their success stories—pushing awareness forward.
What Women Can Do Right Now
If you suspect low testosterone might be impacting your health:
- Document your symptoms – Fatigue, low libido, mood changes, muscle loss, weight gain, brain fog—track them consistently.
- Request specific labs – Total testosterone, free testosterone, SHBG (sex hormone binding globulin), and other hormone markers.
- Seek a second opinion – If your concerns are dismissed, connect with a provider who understands female TRT, such as those in the AlphaMD network.
- Educate yourself – Use credible sources like AlphaMD’s Resource Blog to learn what the latest studies say about testosterone and women’s health.
The Bottom Line
Women deserve the same respect, options, and science-backed treatments as men when it comes to hormone health. The “female TRT backlash” isn’t about safety—it’s about outdated medical thinking that hasn’t caught up to modern evidence.
At AlphaMD, we believe women should have access to the information, lab testing, and medical guidance they need to make informed choices about their hormone health. Because testosterone matters for women, too—and it’s time the medical world caught up.
Frequently Asked Questions About Female TRT
1. Do women naturally produce testosterone?
Yes. Women produce testosterone in their ovaries and adrenal glands. While levels are lower than in men, testosterone plays a key role in energy, mood, libido, muscle mass, and bone health.
2. Why is testosterone therapy for women controversial?
Much of the resistance comes from outdated medical training, lack of FDA-approved testosterone products for women in the U.S., and misconceptions about risks.
3. What symptoms can low testosterone cause in women?
Common symptoms include low energy, decreased libido, mood swings, muscle loss, weight gain, brain fog, and reduced motivation.
4. Is testosterone therapy safe for women?
When prescribed in low, physiologic doses and monitored regularly, testosterone therapy can be safe and effective for women. Most concerns stem from older studies that used much higher doses.
5. How can I find a doctor who will consider TRT?
Look for providers experienced in hormone optimization for women. AlphaMD connects patients with trusted practitioners who understand the science and benefits of female TRT.
6. How quickly will I notice results?
Many women begin to notice improvements in energy, mood, and libido within weeks, but full benefits often take a few months as hormone levels stabilize.
Have a question? Ask us.
At AlphaMD, we're here to help. Feel free to ask us any question you would like about TRT, medical weightloss, ED, or other topics related to men's health. Or take a moment to browse through our past questions.
People are asking...
It seems like its very difficult for many people to get a PCP to write a prescription for testosterone. Is this because there is greater risk of malp...
This is true about the challenging nature of getting a PCP to sign off on TRT, but not for those reasons. TRT is one of the safest treatments out there with one of the lowest malpractice insurance rat... See Full Answer
Do you treat women? And would admitting I've been taking small amounts [10-20mgs/week IM] of my bf's Test (and getting great results) be a barrier to...
We currently have female patients on similar low doses to optimize their hormones. They typically need a bit of Estrogen to keep everything in balance as well as the Test, and to be monitored a bit mo... See Full Answer
Do you foresee patients currently dependent on TRT to sort of be “screwed” at any point due to increased regulations that make it so they can no longe...
I don’t have a crystal ball, but I don’t see that being a problem. Treatment is becoming more prevalent because we are better at recognizing the symptoms, more open about talking about it, and recent ... See Full Answer
Get $30 off your first month’s order
Enter your email address now to receive $30 off your first month’s cost, other discounts, and additional information about TRT.
Legal Disclaimer
This website is a repository of publicly available information and is not intended to form a physician-patient relationship with any individual. The content of this website is for informational purposes only. The information presented on this website is not intended to take the place of your personal physician's advice and is not intended to diagnose, treat, cure, or prevent any disease. Discuss this information with your own physician or healthcare provider to determine what is right for you. All information is intended for your general knowledge only and is not a substitute for medical advice or treatment for specific medical conditions. The information contained herein is presented in summary form only and intended to provide broad consumer understanding and knowledge. The information should not be considered complete and should not be used in place of a visit, phone or telemedicine call, consultation or advice of your physician or other healthcare provider. Only a qualified physician in your state can determine if you qualify for and should undertake treatment.
